Epidemiology
Tyler J. VanderWeele, professor of epidemiology at Harvard University: “Integrating mental health into patient care is key”

Harvard Professor Advocates for Integrated Mental Health Care
What’s Happening?
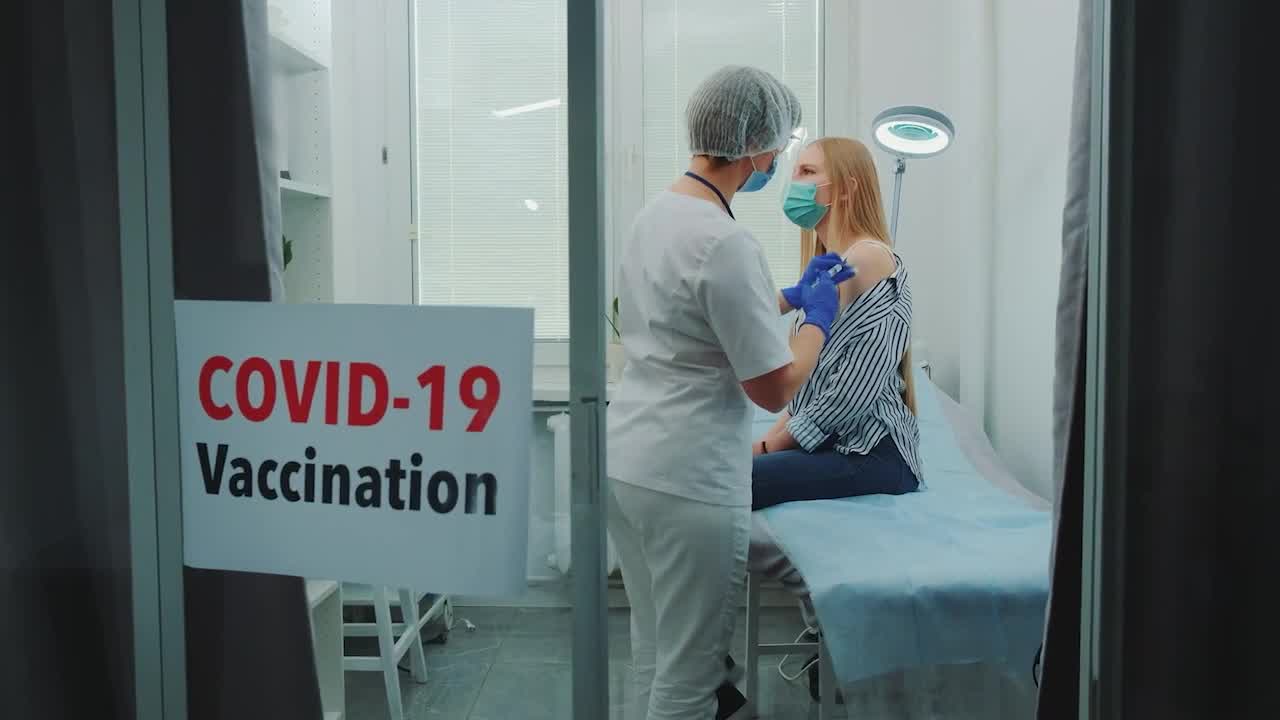
Leading Harvard epidemiologist Tyler J. VanderWeele emphasizes the urgent need for integrating mental health into routine patient care, sparking crucial conversations in healthcare. His insights, shared at a high-profile conference, highlight a paradigm shift in how we approach well-being.
Where Is It Happening?
The discussion took place at a conference organized by UNIR and the Academy of Distinguished Physicians of Madrid, garnering global attention.
When Did It Take Place?
The event occurred recently, though the exact date was not specified. The impact of the professor’s remarks continues to reverberate in the medical community.
How Is It Unfolding?
- VanderWeele stressed the interconnectedness of mental and physical health, advocating for a holistic approach.
- The conference brought together healthcare leaders to rethink traditional patient care models.
- Attendees debated practical strategies for implementing mental health screenings in general practice.
- The event sparked discussions on policy changes needed to support integrated healthcare systems.
- Professionals across sectors expressed growing consensus on the need for systemic change.
Quick Breakdown
- Harvard professor highlights the urgency of mental health integration in healthcare.
- Conference hosted by UNIR and Madrid’s Academy of Distinguished Physicians.
- Call for policy changes to support holistic patient care models.
- Global healthcare leaders explore new strategies for mental and physical health.
Key Takeaways
Ignoring mental health has led to a fragmented healthcare system. VanderWeele argues that addressing mental well-being isn’t optional—it’s essential for treating patients as whole individuals. By integrating mental health into regular care, we can manage chronic conditions more effectively, reduce healthcare costs, and ultimately save lives. The time for change is now, and this shift promises to revolutionize how we understand health.
The biggest hurdle isn’t the science—it’s the will to change how we’ve always done things.
– Dr. Rosa Martinez, Psychiatric Researcher, Madrid University
Final Thought
**VanderWeele’s message is clear: we can’t afford to treat mental and physical health separately anymore. By embracing a unified approach, we unlock better outcomes for patients and a more sustainable future for healthcare. It’s time to see wellness as a whole, not as fragments—because healing should never be piecemeal.**